ASTM F1608-21
(Test Method)Standard Test Method for Microbial Ranking of Porous Packaging Materials (Exposure Chamber Method)
Standard Test Method for Microbial Ranking of Porous Packaging Materials (Exposure Chamber Method)
SIGNIFICANCE AND USE
5.1 The exposure-chamber method is a quantitative procedure for determining the microbial-barrier properties of porous materials under the conditions specified by the test. Data obtained from this test is useful in assessing the relative potential of a particular porous material in contributing to the loss of sterility to the contents of the package versus another porous material. This test method is not intended to predict the performance of a given material in a specific sterile-packaging application. The maintenance of sterility in a particular packaging application will depend on a number of factors, including, but not limited to the following:
5.1.1 The bacterial challenge (number and kinds of microorganisms) that the package will encounter in its distribution and use. This may be influenced by factors such as shipping methods, expected shelf life, geographic location, and storage conditions.
5.1.2 The package design, including factors such as adhesion between materials, the presence or absence of secondary and tertiary packaging, and the nature of the device within the package.
5.1.3 The rate and volume exchange of air that the porous package encounters during its distribution and shelf life. This can be influenced by factors including the free-air volume within the package and pressure changes occurring as a result of transportation, manipulation, weather, or mechanical influences (such as room door closures and HVAC systems).
5.1.4 The microstructure of a porous material which influences the relative ability to adsorb or entrap microorganisms, or both, under different air-flow conditions.
SCOPE
1.1 This test method is used to determine the passage of airborne bacteria through porous materials intended for use in packaging sterile medical devices. This test method is designed to test materials under conditions that result in the detectable passage of bacterial spores through the test material.
1.1.1 A round-robin study was conducted with eleven laboratories participating. Each laboratory tested duplicate samples of six commercially available porous materials to determine the Log Reduction Value (LRV) (see calculation in Section 12). Materials tested under the standard conditions described in this test method returned average values that range from LRV 1.7 to 4.3.
1.1.2 Results of this round-robin study indicate that caution should be used when comparing test data and ranking materials, especially when a small number of sample replicates are used. In addition, further collaborative work (such as described in Practice E691) should be conducted before this test method would be considered adequate for purposes of setting performance standards.
1.2 This test method requires manipulation of microorganisms and should be performed only by trained personnel. The U.S. Department of Health and Human Services publication Biosafety in Microbiological and Biomedical Laboratories (CDC/NIH-HHS Publication No. 84-8395) should be consulted for guidance.
1.3 The values stated in SI units are to be regarded as standard. No other units of measurement are included in this standard.
1.4 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety, health, and environmental practices and determine the applicability of regulatory limitations prior to use.
1.5 This international standard was developed in accordance with internationally recognized principles on standardization established in the Decision on Principles for the Development of International Standards, Guides and Recommendations issued by the World Trade Organization Technical Barriers to Trade (TBT) Committee.
General Information
Relations
Standards Content (Sample)
This international standard was developed in accordance with internationally recognized principles on standardization established in the Decision on Principles for the
Development of International Standards, Guides and Recommendations issued by the World Trade Organization Technical Barriers to Trade (TBT) Committee.
Designation: F1608 − 21
Standard Test Method for
Microbial Ranking of Porous Packaging Materials (Exposure
Chamber Method)
This standard is issued under the fixed designation F1608; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision.Anumber in parentheses indicates the year of last reapproval.A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
1. Scope 1.5 This international standard was developed in accor-
dance with internationally recognized principles on standard-
1.1 This test method is used to determine the passage of
ization established in the Decision on Principles for the
airborne bacteria through porous materials intended for use in
Development of International Standards, Guides and Recom-
packagingsterilemedicaldevices.Thistestmethodisdesigned
mendations issued by the World Trade Organization Technical
to test materials under conditions that result in the detectable
Barriers to Trade (TBT) Committee.
passage of bacterial spores through the test material.
1.1.1 Around-robin study was conducted with eleven labo-
2. Referenced Documents
ratories participating. Each laboratory tested duplicate samples
2.1 ASTM Standards:
of six commercially available porous materials to determine
E691Practice for Conducting an Interlaboratory Study to
theLogReductionValue(LRV)(seecalculationinSection12).
Determine the Precision of a Test Method
Materialstestedunderthestandardconditionsdescribedinthis
testmethodreturnedaveragevaluesthatrangefromLRV1.7to
3. Terminology
4.3.
3.1 Definitions:
1.1.2 Results of this round-robin study indicate that caution
3.1.1 porous packaging material, n—a material used in
should be used when comparing test data and ranking
medical packaging which is intended to provide an environ-
materials,especiallywhenasmallnumberofsamplereplicates
mentalandbiologicalbarrier,whileallowingsufficientairflow
are used. In addition, further collaborative work (such as
to be used in gaseous sterilization methods (for example,
described in Practice E691) should be conducted before this
ethylene oxide, steam, gas plasma).
test method would be considered adequate for purposes of
setting performance standards.
4. Summary of Test Method
1.2 This test method requires manipulation of microorgan-
4.1 Samples of porous materials are subjected to an aerosol
isms and should be performed only by trained personnel. The
of Bacillus atrophaeus spores within an exposure chamber.
U.S. Department of Health and Human Services publication
Spores which pass through the porous sample are collected on
Biosafety in Microbiological and Biomedical Laboratories
membrane filters and enumerated. The LRV is calculated by
(CDC/NIH-HHS Publication No. 84-8395) should be con-
comparing the logarithm of the number of spores passing
sulted for guidance.
throughtheporousmaterialwiththelogarithmofthemicrobial
1.3 The values stated in SI units are to be regarded as
challenge.
standard. No other units of measurement are included in this
4.2 Standard Set of Conditions—This test method specifies
standard.
a standard set of conditions for conducting the exposure
1.4 This standard does not purport to address all of the
chambertestmethod.Astandardsetofconditionsisrequiredto
safety concerns, if any, associated with its use. It is the
enable evaluation of materials between laboratories. The con-
responsibility of the user of this standard to establish appro-
ditions stated in this test method were chosen for several
priate safety, health, and environmental practices and deter-
reasons. First, it is difficult to maintain an aerosol of spores
mine the applicability of regulatory limitations prior to use.
over long periods of time. (Also, if the spore challenge time is
long, the cost of the test increases). Second, to determine the
differences between materials, it is necessary to test the
ThistestmethodisunderthejurisdictionofASTMCommitteeF02onPrimary
Barrier Packaging and is the direct responsibility of Subcommittee F02.15 on
Chemical/Safety Properties. For referenced ASTM standards, visit the ASTM website, www.astm.org, or
Current edition approved Oct. 1, 2021. Published November 2021. Originally contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM
approved in 1995. Last previous edition approved in 2016 as F1608–16. DOI: Standards volume information, refer to the standard’s Document Summary page on
10.1520/F1608-21. the ASTM website.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959. United States
F1608 − 21
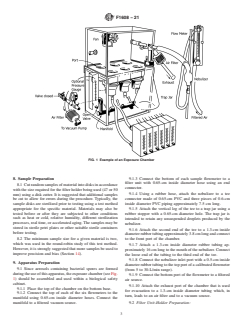
materials under conditions which allow passage of bacterial 6.2 Exposure Chamber, constructed primarily from acrylic
spores. If a material does not allow any passage of spores, all sheeting and consists of two major sections, as illustrated in
that can be stated is that it has better resistance to penetration Fig. 1. The bottom section contains a six-place manifold
than the severity of the challenge conditions. Third, it is connected to six flowmeters, one per port, containing hoses
necessary to have a large spore challenge level to be able to attached to six filtering units. The port to the manifold is
detect the passage of spores through the entire range of attached to a vacuum source. A vacuum gauge is mounted
commercially available porous packaging materials. The stan- between the manifold and the vacuum source. The upper
dard conditions stated in this test method are based upon these chamber contains a fan for dispersion of the bacterial aerosol,
factors. (Additional information may be found in the Refer- aportforattachmentofthenebulizer,aportforexhaustingthe
ences section). However, since many factors influence the chamber, and a plate for attachment of disposable or steriliz-
determination of an appropriate porous material (outlined in ablefilterunits.Thechambermayusedisposablefilterunitsor
5.1.1 – 5.1.4), each user may modify these conditions (that is, reusable filter units, or both.
bacterial challenge, time, flow rate) after first conducting
studiesatthespecifiedstandardconditions.Thestandardsetof 7. Materials
targetparametersforconductingthetestmethodareasfollows:
7.1 Bacillus atrophaeus (ATCC9372), aqueous spore sus-
4.2.1 Flow Rate Through Sample—2.8 L/min.
pension in water.
4.2.2 Exposure Time— 15 min.
7.2 Soybean Casein Digest Agar/ Tryptic Soy Agar—Bottles
4.2.3 Target Microbial Challenge —1×10 colony forming
for pour plates and pre-poured plates (;25 mL in 100 by
units (CFU)/sample port.
15-mm plates) prepared commercially or in accordance with
standard techniques.
5. Significance and Use
7.3 Sterile Cellulose Nitrate Filters, 47 or 50-mm diameter,
5.1 The exposure-chamber method is a quantitative proce-
depending upon filter unit specification, 0.45-µm pore size.
dure for determining the microbial-barrier properties of porous
materials under the conditions specified by the test. Data 7.4 Sterile Bottle-Top Filter Units, (Falcon-type 7104 or
obtained from this test is useful in assessing the relative
filter holders with funnel 310-4000 or equivalent).
potential of a particular porous material in contributing to the
7.5 Glass Nebulizer.
loss of sterility to the contents of the package versus another
7.6 Sterile Forceps.
porous material.This test method is not intended to predict the
performance of a given material in a specific sterile-packaging
7.7 Incubator, 30 to 35°C.
application. The maintenance of sterility in a particular pack-
7.8 Disk Cutter, 47 or 50-mm diameter, depending upon
aging application will depend on a number of factors,
filter unit specification.
including, but not limited to the following:
7.9 Sterile Gloves.
5.1.1 The bacterial challenge (number and kinds of micro-
organisms) that the package will encounter in its distribution
7.10 Sterile Syringe, 3-cm with needle or micropipette.
and use. This may be influenced by factors such as shipping
7.11 Sterile Pipettes, to deliver 0.1, 1, 10, and 25 mL.
methods, expected shelf life, geographic location, and storage
7.12 Blender, with sterile ⁄2-pt jar(s).
conditions.
5.1.2 The package design, including factors such as adhe-
7.13 Vortex Mixer.
sion between materials, the presence or absence of secondary
7.14 Vacuum Pump, with air filter.
and tertiary packaging, and the nature of the device within the
7.15 NIST Traceable Calibrated Timer.
package.
5.1.3 The rate and volume exchange of air that the porous
7.16 NIST Traceable Calibrated Flowmeters—Onepressure
package encounters during its distribution and shelf life. This
flowmeter with a range from 5 to 30 L/min; six vacuum
can be influenced by factors including the free-air volume
flowmeters each with a range from 1.0 to 5.0 L/min.
within the package and pressure changes occurring as a result
7.17 Sterile Petri Plates.
of transportation, manipulation, weather, or mechanical influ-
7.18 Sterile Water, 100 and 9.9-mLaliquots, or other appro-
ences (such as room door closures and HVAC systems).
priate volumes for membrane grinding and dilutions.
5.1.4 The microstructure of a porous material which influ-
ences the relative ability to adsorb or entrap microorganisms,
7.19 Hoses and Piping— See Section 9 for lengths and
or both, under different air-flow conditions.
diameters.
7.20 Rubber Stoppers with Holes—See Section 9 for sizes.
6. Apparatus
7.21 Trap Jar.
6.1 This procedure should be conducted in a microbiologi-
7.22 NIST Traceable Calibrated Vacuum Gauge.
cal laboratory by trained personnel. As a result, it is assumed
thatbasicmicrobiologicalequipmentandsuppliesforconduct-
7.23 Compressed Air Source, with air filter.
ing routine microbiological manipulations (that is, standard
7.24 Biocontainment Hood.
plate counts, sterilization with an autoclave, and so forth) will
be available. 7.25 Chlorine Bleach, or suitable sporocide.
F1608 − 21
FIG. 1 Example of an Exposure Chamber
8. Sample Preparation 9.1.3 Connect the bottom of each sample flowmeter to a
filter unit with 0.65-cm inside diameter hose using an end
8.1 Cutrandomsamplesofmaterialintodisksinaccordance
connector.
with the size required for the filter holder being used (47 or 50
9.1.4 Using a rubber hose, attach the nebulizer to a tee
mm) using a disk cutter. It is suggested that additional samples
connector made of 0.65-cm PVC and three pieces of 0.6-cm
be cut to allow for errors during the procedure. Typically, the
inside diameter PVC piping approximately 7.5 cm long.
sample disks are sterilized prior to testing using a test method
appropriate for the specific material. Materials may also be
9.1.5 Attach the vertical leg of the tee to a trap jar using a
tested before or after they are subjected to other conditions
rubber stopper with a 0.65-cm diameter hole. The trap jar is
such as heat or cold, relative humidity, different sterilization
intended to retain any unsuspended droplets produced by the
processes, real time, or accelerated aging.The samples may be
nebulizer.
stored in sterile petri plates or other suitable sterile containers
9.1.6 Attach the second end of the tee to a 1.3-cm inside
before testing.
diameterrubbertubingapproximately3.8cmlongandconnect
8.2 The minimum sample size for a given material is two, to the front port of the chamber.
which was used in the round-robin study of this test method.
9.1.7 Attach a 1.3-cm inside diameter rubber tubing ap-
However,itisstronglysuggestedthatmoresamplesbeusedto
proximately16cmlongtothemouthofthenebulizer.Connect
improve precision and bias (Section 14).
the loose end of the tubing to the third end of the tee.
9.1.8 Connect the nebulizer inlet port with a 0.5-cm inside
9. Apparatus Preparation
diameterrubbertubingtothetopportofacalibratedflowmeter
9.1 Since aerosols containing bacterial spores are formed
(from 5 to 30-L/min range).
duringtheuseofthisapparatus,theexposurechamber(seeFig.
9.1.9 Connect the bottom port of the flowmeter to a filtered
1) should be assembled and used within a biological safety
air source.
cabinet.
9.1.10 Attach the exhaust port of the chamber that is used
9.1.1 Place the top of the chamber on the bottom base.
for evacuation to a 1.3-cm inside diameter tubing which, in
9.1.2 Connect the top of each of the six flowmeters to the
turn, leads to an air filter and to a vacuum source.
manifold using 0.65-cm inside diameter hoses. Connect the
manifold to a filtered vacuum source. 9.2 Filter Unit-Holder Preparation:
F1608 − 21
9.2.1 Wrap the non-sterile sterilizable filter unit in a steril- of 3.0 mLat a concentration of 5×10 spores/mLis necessary
izable wrap. toachieveachallengeof1×10 CFU(60.5log)perportin15
9.2.2 Sterilize the filter units as specified by the manufac- min.
turer. Presterilized filter units do not need to be resterilized. 10.1.5 Turn on the chamber fan.
10.1.6 Adjust port flowmeters to 2.8 L/min. It is important
10. Apparatus Validation that all ports be set to the same flow and monitored during the
exposure period. Before adjusting each flowmeter, open each
10.1 The test apparatus (see Fig. 1) must be validated for
valve completely, then slowly open the vacuum and fine adjust
bacterialchallengetoeachport.Thisstepshouldbeperformed
until the desired flow is achieved.
upon first use of the chamber and a minimum of three runs
10.1.7 Adjust the nebulizer flow rate as recommended by
should be conducted. The following description outlines the
6 the nebulizer manufacturer to produce droplets that are within
validation of the test procedure for a challenge of 1×10
the appropriate particle size range. When using the DeVilbiss
colonyformingunits(CFU)perportin15minataflowrateof
#40 nebulizer, a flow rate of 8.5 L/min is used.
2.8L/min.Iftestingistobeconductedusingotherparameters,
10.1.8 Immediately start the 15-min timer. At regular
a validation should be conducted using those parameters.
intervals, observe and adjust (if necessary) all flowmeters to
10.1.1 Place the sterile filtering apparatus in a biological
maintain the appropriate flow rate settings during the 15-min
safety cabinet.
test period.
10.1.2 Asepticallypreparesixfilterunitsbyplacingasterile
10.1.9 After exposure, turn off the vacuum, the fan, and the
0.45-µm membrane filter on the base of each filter unit using
air flow to the nebulizer. Open the filtered exhaust port at the
sterile forceps and gloves (Fig. 2B).
back of the chamber.
10.1.3 Attach the top of each filter unit to the bottom of the
10.1.10 Evacuate the chamber for 15 min by connecting the
exposure chamber.Then
...
This document is not an ASTM standard and is intended only to provide the user of an ASTM standard an indication of what changes have been made to the previous version. Because
it may not be technically possible to adequately depict all changes accurately, ASTM recommends that users consult prior editions as appropriate. In all cases only the current version
of the standard as published by ASTM is to be considered the official document.
Designation: F1608 − 16 F1608 − 21
Standard Test Method for
Microbial Ranking of Porous Packaging Materials (Exposure
Chamber Method)
This standard is issued under the fixed designation F1608; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
1. Scope
1.1 This test method is used to determine the passage of airborne bacteria through porous materials intended for use in packaging
sterile medical devices. This test method is designed to test materials under conditions that result in the detectable passage of
bacterial spores through the test material.
1.1.1 A round-robin study was conducted with eleven laboratories participating. Each laboratory tested duplicate samples of six
commercially available porous materials to determine the Log Reduction Value (LRV) (see calculation in Section 12). Materials
tested under the standard conditions described in this test method returned average values that range from LRV 1.7 to 4.3.
1.1.2 Results of this round-robin study indicate that caution should be used when comparing test data and ranking materials,
especially when a small number of sample replicates are used. In addition, further collaborative work (such as described in Practice
E691) should be conducted before this test method would be considered adequate for purposes of setting performance standards.
1.2 This test method requires manipulation of microorganisms and should be performed only by trained personnel. The U.S.
Department of Health and Human Services publication Biosafety in Microbiological and Biomedical Laboratories (CDC/NIH-
HHS Publication No. 84-8395) should be consulted for guidance.
1.3 The values stated in SI units are to be regarded as standard. No other units of measurement are included in this standard.
1.4 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility
of the user of this standard to establish appropriate safety safety, health, and healthenvironmental practices and determine the
applicability of regulatory limitations prior to use.
1.5 This international standard was developed in accordance with internationally recognized principles on standardization
established in the Decision on Principles for the Development of International Standards, Guides and Recommendations issued
by the World Trade Organization Technical Barriers to Trade (TBT) Committee.
2. Referenced Documents
2.1 ASTM Standards:
E691 Practice for Conducting an Interlaboratory Study to Determine the Precision of a Test Method
This test method is under the jurisdiction of ASTM Committee F02 on FlexiblePrimary Barrier Packaging and is the direct responsibility of Subcommittee F02.15 on
Chemical/Safety Properties.
Current edition approved May 1, 2016Oct. 1, 2021. Published June 2016November 2021. Originally approved in 1995. Last previous edition approved in 20092016 as
F1608 – 00 (2009).F1608 – 16. DOI: 10.1520/F1608-16.10.1520/F1608-21.
For referenced ASTM standards, visit the ASTM website, www.astm.org, or contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM Standards
volume information, refer to the standard’s Document Summary page on the ASTM website.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959. United States
F1608 − 21
3. Terminology
3.1 Definitions:
3.1.1 porous packaging material, n—a material used in medical packaging which is intended to provide an environmental and
biological barrier, while allowing sufficient air flow to be used in gaseous sterilization methods (for example, ethylene oxide,
steam, gas plasma).
4. Summary of Test Method
4.1 Samples of porous materials are subjected to an aerosol of Bacillus atrophaeus spores within an exposure chamber. Spores
which pass through the porous sample are collected on membrane filters and enumerated. The LRV is calculated by comparing the
logarithm of the number of spores passing through the porous material with the logarithm of the microbial challenge.
4.2 Standard Set of Conditions—This test method specifies a standard set of conditions for conducting the exposure chamber test
method. A standard set of conditions is required to enable evaluation of materials between laboratories. The conditions stated in
this test method were chosen for several reasons. First, it is difficult to maintain an aerosol of spores over long periods of time.
(Also, if the spore challenge time is long, the cost of the test increases). Second, to determine the differences between materials,
it is necessary to test the materials under conditions which allow passage of bacterial spores. If a material does not allow any
passage of spores, all that can be stated is that it has better resistance to penetration than the severity of the challenge conditions.
Third, it is necessary to have a large spore challenge level to be able to detect the passage of spores through the entire range of
commercially available porous packaging materials. The standard conditions stated in this test method are based upon these factors.
(Additional information may be found in the References section). However, since many factors influence the determination of an
appropriate porous material (outlined in 5.1.1 – 5.1.4), each user may modify these conditions (that is, bacterial challenge, time,
flow rate) after first conducting studies at the specified standard conditions. The standard set of target parameters for conducting
the test method are as follows:
4.2.1 Flow Rate Through Sample—2.8 L/min.
4.2.2 Exposure Time— 15 min.
4.2.3 Target Microbial Challenge —1 × 10 colony forming units (CFU)/sample port.
5. Significance and Use
5.1 The exposure-chamber method is a quantitative procedure for determining the microbial-barrier properties of porous materials
under the conditions specified by the test. Data obtained from this test is useful in assessing the relative potential of a particular
porous material in contributing to the loss of sterility to the contents of the package versus another porous material. This test
method is not intended to predict the performance of a given material in a specific sterile-packaging application. The maintenance
of sterility in a particular packaging application will depend on a number of factors, including, but not limited to the following:
5.1.1 The bacterial challenge (number and kinds of microorganisms) that the package will encounter in its distribution and use.
This may be influenced by factors such as shipping methods, expected shelf life, geographic location, and storage conditions.
5.1.2 The package design, including factors such as adhesion between materials, the presence or absence of secondary and tertiary
packaging, and the nature of the device within the package.
5.1.3 The rate and volume exchange of air that the porous package encounters during its distribution and shelf life. This can be
influenced by factors including the free-air volume within the package and pressure changes occurring as a result of transportation,
manipulation, weather, or mechanical influences (such as room door closures and HVAC systems).
5.1.4 The microstructure of a porous material which influences the relative ability to adsorb or entrap microorganisms, or both,
under different air-flow conditions.
6. Apparatus
6.1 This procedure should be conducted in a microbiological laboratory by trained personnel. As a result, it is assumed that basic
microbiological equipment and supplies for conducting routine microbiological manipulations (that is, standard plate counts,
sterilization with an autoclave, and so forth) will be available.
F1608 − 21
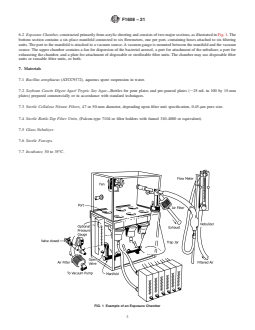
6.2 Exposure Chamber, constructed primarily from acrylic sheeting and consists of two major sections, as illustrated in Fig. 1. The
bottom section contains a six-place manifold connected to six flowmeters, one per port, containing hoses attached to six filtering
units. The port to the manifold is attached to a vacuum source. A vacuum gauge is mounted between the manifold and the vacuum
source. The upper chamber contains a fan for dispersion of the bacterial aerosol, a port for attachment of the nebulizer, a port for
exhausting the chamber, and a plate for attachment of disposable or sterilizable filter units. The chamber may use disposable filter
units or reusable filter units, or both.
7. Materials
7.1 Bacillus atrophaeus (ATCC9372), aqueous spore suspension in water.
7.2 Soybean Casein Digest Agar/ Tryptic Soy Agar—Bottles for pour plates and pre-poured plates (;25 mL in 100 by 15-mm
plates) prepared commercially or in accordance with standard techniques.
7.3 Sterile Cellulose Nitrate Filters, 47 or 50-mm diameter, depending upon filter unit specification, 0.45-μm pore size.
7.4 Sterile Bottle-Top Filter Units, (Falcon-type 7104 or filter holders with funnel 310-4000 or equivalent).
7.5 Glass Nebulizer.
7.6 Sterile Forceps.
7.7 Incubator, 30 to 35°C.
FIG. 1 Example of an Exposure Chamber
F1608 − 21
7.8 Disk Cutter, 47 or 50-mm diameter, depending upon filter unit specification.
7.9 Sterile Gloves.
7.10 Sterile Syringe, 3-cm with needle or micropipette.
7.11 Sterile Pipettes, to deliver 0.1, 1, 10, and 25 mL.
7.12 Blender, with sterile ⁄2-pt jar(s).
7.13 Vortex Mixer.
7.14 Vacuum Pump, with air filter.
7.15 NIST Traceable Calibrated Timer.
7.16 NIST Traceable Calibrated Flowmeters—One pressure flowmeter with a range from 5 to 30 L/min; six vacuum flowmeters
each with a range from 1.0 to 5.0 L/min.
7.17 Sterile Petri Plates.
7.18 Sterile Water, 100 and 9.9-mL aliquots, or other appropriate volumes for membrane grinding and dilutions.
7.19 Hoses and Piping— See Section 9 for lengths and diameters.
7.20 Rubber Stoppers with Holes—See Section 9 for sizes.
7.21 Trap Jar.
7.22 NIST Traceable Calibrated Vacuum Gauge.
7.23 Compressed Air Source, with air filter.
7.24 Biocontainment Hood.
7.25 Chlorine Bleach, or suitable sporocide.
8. Sample Preparation
8.1 Cut random samples of material into disks in accordance with the size required for the filter holder being used (47 or 50 mm)
using a disk cutter. It is suggested that additional samples be cut to allow for errors during the procedure. Typically, the sample
disks are sterilized prior to testing using a test method appropriate for the specific material. Materials may also be tested before
or after they are subjected to other conditions such as heat or cold, relative humidity, different sterilization processes, real time,
or accelerated aging. The samples may be stored in sterile petri plates or other suitable sterile containers before testing.
8.2 The minimum sample size for a given material is two, which was used in the round-robin study of this test method. However,
it is strongly suggested that more samples be used to improve precision and bias (Section 14).
F1608 − 21
9. Apparatus Preparation
9.1 Since aerosols containing bacterial spores are formed during the use of this apparatus, the exposure chamber (see Fig. 1)
should be assembled and used within a biological safety cabinet.
9.1.1 Place the top of the chamber on the bottom base.
9.1.2 Connect the top of each of the six flowmeters to the manifold using 0.65-cm inside diameter hoses. Connect the manifold
to a filtered vacuum source.
9.1.3 Connect the bottom of each sample flowmeter to a filter unit with 0.65-cm inside diameter hose using an end connector.
9.1.4 Using a rubber hose, attach the nebulizer to a tee connector made of 0.65-cm PVC and three pieces of 0.6-cm inside diameter
PVC piping approximately 7.5 cm long.
9.1.5 Attach the vertical leg of the tee to a trap jar using a rubber stopper with a 0.65-cm diameter hole. The trap jar is intended
to retain any unsuspended droplets produced by the nebulizer.
9.1.6 Attach the second end of the tee to a 1.3-cm inside diameter rubber tubing approximately 3.8 cm long and connect to the
front port of the chamber.
9.1.7 Attach a 1.3-cm inside diameter rubber tubing approximately 16 cm long to the mouth of the nebulizer. Connect the loose
end of the tubing to the third end of the tee.
9.1.8 Connect the nebulizer inlet port with a 0.5-cm inside diameter rubber tubing to the top port of a calibrated flowmeter (from
5 to 30-L/min range).
9.1.9 Connect the bottom port of the flowmeter to a filtered air source.
9.1.10 Attach the exhaust port of the chamber that is used for evacuation to a 1.3-cm inside diameter tubing which, in turn, leads
to an air filter and to a vacuum source.
9.2 Filter Unit-Holder Preparation:
9.2.1 Wrap the non-sterile sterilizable filter unit in a sterilizable wrap.
9.2.2 Sterilize the filter units as specified by the manufacturer. Presterilized filter units do not need to be resterilized.
10. Apparatus Validation
10.1 The test apparatus (see Fig. 1) must be validated for bacterial challenge to each port. This step should be performed upon
first use of the chamber and a minimum of three runs should be conducted. The following description outlines the validation of
the test procedure for a challenge of 1 × 10 colony forming units (CFU) per port in 15 min at a flow rate of 2.8 L/min. If testing
is to be conducted using other parameters, a validation should be conducted using those parameters.
10.1.1 Place the sterile filtering apparatus in a biological safety cabinet.
10.1.2 Aseptically prepare six filter units by placing a sterile 0.45-μm membrane filter on the base of each filter unit using sterile
forceps and gloves (Fig. 2B).
10.1.3 Attach the top of each filter unit to the bottom of the exposure chamber. Then attach each filter unit to its respective
flowmeter.
10.1.4 Dispense 3.0 mL of the spore suspension into the nebulizer. When using the DeVilbiss #40 nebulizer, a volume of 3.0 mL
7 6
at a concentration of 5 × 10 spores/mL is necessary to achieve a challenge of 1 × 10 CFU (60.5 log) per port in 15 min.
10.1.5 Turn on the chamber fan.
F1608 − 21
FIG. 2 Sample and Control Material Setup
10.1.6 Adjust port flowmeters to 2.8 L/min. It is important that all ports be set to the same flow and monitored during the exposur
...








Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.